- When will the Nevada Medicaid dental benefits transition to LIBERTY Dental Plan of Nevada?
- Where do I submit claims for Nevada Medicaid members after January 1, 2018?
- Does LIBERTY accept NEA FastAttach?
- Will LIBERTY honor services previously approved for Nevada Medicaid members?
- Who is responsible for any Nevada Medicaid member’s unpaid claims for dates of service prior to the January 1, 2018 roll out?
- Are referrals for specialty care required?
- When is prior authorization necessary?
- Is prior authorization required for a general dentist to refer a member for an orthodontic evaluation?
- Does the member ID card guarantee eligibility?
- What is LIBERTY’s turnaround time for prior authorization and claims processing?
- What is LIBERTY’s turnaround time for prior authorization and claims processing?
- What if my patient is the beneficiary or member of more than one plan? How is Coordination of Benefits handled for the Nevada Medicaid program?
- How can I sign up for LIBERTY’s Provider Portal?
- How do I obtain LIBERTY’s Benefit Plans?
- Does LIBERTY pay on prep date or delivery date?
- Does LIBERTY offer training for dental providers?
- How do I receive electronic claims payment?
- Will providers have access to claims history for Nevada Medicaid members?
- How can I obtain a copy of an eligibility roster?
- Does a member have to appear on my roster in order to be eligible to receive treatment?
When will the Nevada Medicaid dental benefits transition to LIBERTY Dental Plan of Nevada?
LIBERTY Dental Plan of Nevada (LIBERTY) will be the new Dental Benefits Administrator effective January 1, 2018 to serve members enrolled in a Managed Care Organization (MCO) in Washoe and Clark counties.
Where do I submit claims for Nevada Medicaid members after January 1, 2018?
All dental claims for managed care members for dates of service on or after January 1, 2018, should be sent to LIBERTY electronically via EDI (Payor ID is CX083), LIBERTY’s web portal at:
- www.libertydentalplan.com/NVMedicaid
 or you can send them directly to:
or you can send them directly to: -
- LIBERTY Dental Plan of Nevada
- PO Box 401086
- Las Vegas, NV 89140
Claims submitted to Fee-For-Service (FFS) Nevada Medicaid for dates of service on or after January 1, 2018 will be denied with edit 0463 (Enrolled in DBA)
All dental claims for managed care members for dates of services between July 1, 2017 and December 31, 2017, should be sent to Fee-For-Service (FFS) Nevada Medicaid. Claims within this date range received after January 1, 2018 will continue to be processed by to Fee-For-Service (FFS) Nevada Medicaid.
Does LIBERTY accept NEA FastAttach?
Yes, LIBERTY accepts NEA FastAttach. Below is the contact information:
- National Electronic Attachment, Inc.
- (800) 782-5150
- www.nea-fast.com

Will LIBERTY honor services previously approved for Nevada Medicaid members?
LIBERTY will ensure continuity of care for Nevada Medicaid members and will honor prior authorizations for services approved by the previous carrier for up to 120 days following the January 1, 2018 effective date with LIBERTY.
Who is responsible for any Nevada Medicaid member’s unpaid claims for dates of service prior to the January 1, 2018 roll out?
The former dental carrier is responsible to pay claims for any treatment rendered prior to the January 1, 2018 effective date with LIBERTY.
Are referrals for specialty care required?
Yes. Specialty care referrals are required for endodontists, oral surgeons or periodontists.
When is prior authorization necessary?
Prior authorization applies to general dentists and specialists for certain covered procedures. Please refer to the Nevada Medicaid benefit schedule for services that require prior authorization.
Is prior authorization required for a general dentist to refer a member for an orthodontic evaluation?
In all areas of Nevada, orthodontic coverage is provided through the Fee for Service (FFS) benefit plan and requires a dentist’s referral. Prior authorization requests and claims for orthodontics must be submitted to Nevada Medicaid, not LIBERTY.
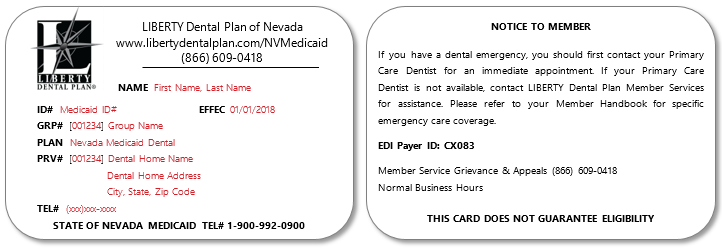
Does the member ID card guarantee eligibility?
No. You must verify eligibility for each member prior to their appointment. Real time eligibility can be verified through LIBERTY at the following link:
Visiting the Provider Portal at: www.libertydentalplan.com/NVMedicaid 
Sample of the ID card
What is LIBERTY’s turnaround time for prior authorization and claims processing?
Our average turnaround times are:
- Prior authorizations - 5 business days of receipt.
- Clean electronic claims - 15 business days
- Clean paper claims - 20 business days
What is the claim filing deadline?
Claims may be submitted for payment up to 180 days following the date of service for in-state providers. Out-of-state providers will have up to 365 days following the date services were rendered. However, LIBERTY recommends that you submit claims for completed treatment either daily or weekly.
What if my patient is the beneficiary or member of more than one plan? How is Coordination of Benefits handled for the Nevada Medicaid program?
The Provider Reference Guide contains detailed information about how Coordination of Benefits occurs when one of the plans is Nevada Medicaid. In general, Nevada Medicaid is the payer of last resort and is secondary to most other plans.
How can I sign up for LIBERTY’s Provider Portal?
Please visit: www.libertydentalplan.com/NVMedicaid  to register as a new user.
Your office’s “Access Code” and “Office Number” will be required to register and are included in your LIBERTY Welcome letter.
to register as a new user.
Your office’s “Access Code” and “Office Number” will be required to register and are included in your LIBERTY Welcome letter.
Please contact LIBERTY’s online administrator at 1.888.700.0643 or send an e-mail to: support@libertydentalplan.com if you are unable to locate your login information.
How do I obtain LIBERTY’s Benefit Plans?
You may obtain a copy by logging in to LIBERTY’s secure provider portal at:
Does LIBERTY pay on prep date or delivery date?
Claims should be submitted reflecting the delivery date of fixed and/or removable appliances.
Does LIBERTY offer training for dental providers?
Yes, we offer providers training during orientation; in addition, training documents can be referenced on our website at:
How do I receive electronic claims payment?
LIBERTY encourages providers to sign up for EFT (direct deposit) so that you receive your payments faster. The EFT form can be obtained on our website at:
Will providers have access to claims history for Nevada Medicaid members?
Yes.
How can I obtain a copy of an eligibility roster?
You can verify real-time eligibility by signing on to our website at: www.libertydentalplan.com/NVMedicaid  and select My Member.
Please refer to our User Web Portal guide for additional information.
and select My Member.
Please refer to our User Web Portal guide for additional information.
Does a member have to appear on my roster in order to be eligible to receive treatment?
Yes. Your office can verify real-time eligibility on our web portal. Please select My Members to ensure that members are assigned to your office before providing treatment.